what to do if you get shot by a gun
| Gunshot wound | |
|---|---|
 | |
| Male skull showing bullet exit wound on parietal bone, 1950s. | |
| Specialty | Trauma surgery |
| Symptoms | Pain, deformity, bleeding[one] [2] |
| Complications | PTSD, lead poisoning, nerve injury,[ane] [2] [3] wound infection, sepsis, brain impairment, gangrene, disability, amputation[iv] |
| Causes | Firearm, Gun |
| Risk factors | Illegal drug trade, ignorance of firearm safety, substance misuse including alcohol, mental wellness problems, firearm laws, social and economical differences[5] [six] |
| Prevention | Firearm safety, not being involved in offense[7] [viii] |
| Treatment | Trauma care[nine] |
| Frequency | one one thousand thousand (interpersonal violence in 2015)[10] |
| Deaths | 251,000 (2016)[5] |
A gunshot wound (GSW) is concrete trauma caused by a projectile from a firearm, air gun or other type of guns.[xi] [12] Damage may include haemorrhage, broken bones, organ damage, infection of the wound, loss of the ability to motion office of the body and, in more severe cases, death.[2] Harm depends on the role of the body hitting, the path the bullet follows through the body, and the type and speed of the bullet.[12] Long-term complications can include pb poisoning and mail-traumatic stress disorder (PTSD).[1] [2] [13]
Factors that determine rates of firearm violence vary by country.[5] These factors may include the illegal drug trade, admission to firearms, substance misuse including alcohol, mental health issues, firearm laws, and social and economic differences.[5] [vi] Where guns are more common, altercations more than often terminate in death.[14]
Before direction begins information technology should exist verified the area is safety.[9] This is followed by stopping major haemorrhage, then assessing and supporting the airway, breathing, and circulation.[9] Firearm laws, peculiarly background checks and permit to purchase, decrease the adventure of expiry from firearms.[7] Safer firearm storage may subtract the hazard of firearm-related deaths in children.[viii]
In 2015, about a one thousand thousand gunshot wounds occurred from interpersonal violence.[10] In 2016, firearms resulted in 251,000 deaths globally, up from 209,000 in 1990.[5] Of these deaths 161,000 (64%) were the consequence of set on, 67,500 (27%) were the effect of suicide, and 23,000 (9%) were accidents.[5] In the United states of america, guns resulted in most 40,000 deaths in 2017.[fifteen] Firearm-related deaths are nigh mutual in males between the ages of 20 to 24 years.[5] Economic costs due to gunshot wounds take been estimated at US$140 billion a year in the Usa.[16]
Signs and symptoms [edit]
Trauma from a gunshot wound varies widely based on the bullet, velocity, mass, entry point, trajectory, afflicted anatomy, and leave point. Gunshot wounds can exist particularly devastating compared to other penetrating injuries because the trajectory and fragmentation of bullets can be unpredictable afterward entry. Moreover, gunshot wounds typically involve a large degree of nearby tissue disruption and destruction acquired by the physical effects of the projectile correlated with the bullet velocity classification.[17]
The immediate damaging consequence of a gunshot wound is typically severe bleeding with the potential for hypovolemic daze, a condition characterized by inadequate delivery of oxygen to vital organs.[18] In the instance of traumatic hypovolemic shock, this failure of adequate oxygen delivery is due to claret loss, as blood is the means of delivering oxygen to the body'south constituent parts. Devastating effects can event when a bullet strikes a vital organ such as the eye, lungs or liver, or amercement a component of the cardinal nervous organisation such as the spinal cord or brain.[eighteen]
Mutual causes of death following gunshot injury include bleeding, low oxygen caused past pneumothorax, catastrophic injury to the centre and major claret vessels, and damage to the brain or central nervous organization. Non-fatal gunshot wounds frequently have mild to severe long-lasting furnishings, typically some class of major disfigurement such as amputation because of a severe os fracture and may cause permanent disability. A sudden claret gush may take effect immediately from a gunshot wound if a bullet directly damages larger blood vessels, peculiarly arteries.
Pathophysiology [edit]
The degree of tissue disruption caused by a projectile is related to the cavitation the projectile creates as it passes through tissue. A bullet with sufficient energy will have a cavitation outcome in addition to the penetrating track injury. As the bullet passes through the tissue, initially crushing then lacerating, the infinite left forms a cavity; this is chosen the permanent cavity. College-velocity bullets create a force per unit area wave that forces the tissues away, creating not merely a permanent cavity the size of the caliber of the bullet just a temporary crenel or secondary cavity, which is frequently many times larger than the bullet itself.[xix] The temporary cavity is the radial stretching of tissue around the bullet's wound track, which momentarily leaves an empty space caused past high pressures surrounding the projectile that accelerate material abroad from its path.[eighteen] The extent of cavitation, in plow, is related to the following characteristics of the projectile:
- Kinetic energy: KE = one/2mv 2 (where m is mass and v is velocity). This helps to explain why wounds produced past projectiles of higher mass and/or higher velocity produce greater tissue disruption than projectiles of lower mass and velocity. The velocity of the bullet is a more than of import determinant of tissue injury. Although both mass and velocity contribute to the overall energy of the projectile, the energy is proportional to the mass while proportional to the square of its velocity. As a result, for abiding velocity, if the mass is doubled, the energy is doubled; however, if the velocity of the bullet is doubled, the free energy increases four times. The initial velocity of a bullet is largely dependent on the firearm. The US war machine commonly uses 5.56-mm bullets, which accept a relatively low mass as compared with other bullets; all the same, the speed of these bullets is relatively fast. As a consequence, they produce a larger amount of kinetic energy, which is transmitted to the tissues of the target.[19] [20] The size of the temporary cavity is approximately proportional to the kinetic energy of the bullet and depends on the resistance of the tissue to stress.[18] Cage energy, which is based on muzzle velocity, is often used for ease of comparison.
- Yaw: Handgun bullets volition generally travel in a relatively straight line or make one plough if a bone is hit. Upon travel through deeper tissue, high-free energy rounds may become unstable as they decelerate, and may tumble (pitch and yaw) every bit the energy of the projectile is absorbed, causing stretching and trigger-happy of the surrounding tissue.[19]
- Fragmentation: Most commonly, bullets do not fragment, and secondary damage from fragments of shattered os is a more common complexity than bullet fragments.[19]
Diagnosis [edit]
Classification [edit]
Gunshot wounds are classified according to the speed of the projectile using the Gustilo open fracture classification:
- Low-velocity: Less than 1,100 ft/s (340 chiliad/due south)
Low velocity wounds are typical of minor caliber handguns and display wound patterns similar Gustilo Anderson Type one or two wounds
- Medium-velocity: Between i,200 ft/south (340 m/s) and two,000 ft/due south (610 m/s)
These are more typical of shotgun blasts or higher caliber handguns like magnums. The risk of infection from these types of wounds tin can vary depending on the blazon and design of bullets fired likewise every bit the distance from the firearm.
- High-velocity: Between 2,000 ft/s (610 chiliad/s) and 3,500 ft/s (i,100 1000/s)
Usually acquired by powerful assault or hunting rifles and usually brandish wound design similar to Gustilo Anderson Type three wounds. The run a risk of infection is especially loftier due to the big surface area of injury and destroyed tissue.[21]
Bullets from handguns are sometimes less than ane,000 ft/s (300 thousand/s) but with modern pistol loads, they usually are slightly higher up 1,000 ft/s (300 m/s), while bullets from most modern rifles exceed 2,500 ft/s (760 one thousand/s). Ane recently developed class of firearm projectiles is the hyper-velocity bullet, such cartridges are usually either wildcats made for achieving such high speed or purpose built mill ammunition with the same goal in heed. Examples of hyper velocity cartridges include the .220 Swift, .17 Remington and .17 Mach Iv cartridges. The US armed forces commonly uses 5.56mm bullets, which have a relatively low mass equally compared with other bullets (forty-62 grains); even so, the speed of these bullets is relatively fast (Approximately 2,800 ft/s (850 m/s), placing them in the high velocity category). Equally a result, they produce a larger amount of kinetic free energy, which is transmitted to the tissues of the target.[19] However, one must remember that loftier kinetic energy does not necessarily equate to loftier stopping ability, as incapacitation usually results from remote wounding effects such every bit bleeding, rather than raw energy transfer. Loftier energy does indeed consequence in more than tissue disruption, which plays a role in incapacitation, simply other factors such as wound size and shot placement play as big of, if not a bigger role in stopping power and thus, effectiveness. Muzzle velocity does not consider the effect of aerodynamic drag on the flight of the bullet for the sake of ease of comparison.
Prevention [edit]
Medical organizations in the United States recommend a criminal background check being held before a person buys a gun and that a person who has convictions for crimes of violence should not exist permitted to buy a gun.[15] Safe storage of firearms is recommended, as well equally meliorate mental health care and removal of guns from those at hazard of suicide.[fifteen] In an effort to prevent mass shootings greater regulations on guns that can rapidly fire many bullets is recommended.[15]
Direction [edit]
Initial assessment for a gunshot wound is approached in the same way as other acute trauma using the avant-garde trauma life support (ATLS) protocol.[22] These include:
- A) Airway - Assess and protect airway and potentially the cervical spine
- B) Breathing - Maintain adequate ventilation and oxygenation
- C) Circulation - Appraise for and control bleeding to maintain organ perfusion including focused assessment with sonography for trauma (FAST)
- D) Disability - Perform basic neurological exam including Glasgow Coma Scale (GCS)
- Eastward) Exposure - Expose entire trunk and search for whatsoever missed injuries, entry points, and exit points while maintaining trunk temperature
Depending on the extent of injury, management can range from urgent surgical intervention to observation. As such, any history from the scene such equally gun type, shots fired, shot management and distance, claret loss on scene, and pre-hospital vitals signs can be very helpful in directing management. Unstable people with signs of bleeding that cannot be controlled during the initial evaluation require immediate surgical exploration in the operating room.[22] Otherwise, management protocols are generally dictated by anatomic entry bespeak and anticipated trajectory.
Neck [edit]
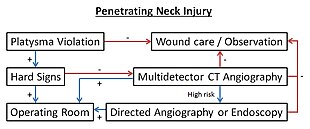
Penetrating neck injury protocol.[23]
A gunshot wound to the neck tin be specially dangerous because of the high number of vital anatomical structures contained inside a small space. The neck contains the larynx, trachea, pharynx, esophagus, vasculature (carotid, subclavian, and vertebral arteries; jugular, brachiocephalic, and vertebral veins; thyroid vessels), and nervous system anatomy (spinal string, cranial nerves, peripheral nerves, sympathetic chain, brachial plexus). Gunshots to the neck can thus cause severe haemorrhage, airway compromise, and nervous system injury.[24]
Initial cess of a gunshot wound to the cervix involves non-probing inspection of whether the injury is a penetrating neck injury (PNI), classified past violation of the platysma muscle.[24] If the platysma is intact, the wound is considered superficial and only requires local wound care. If the injury is a PNI, surgery should be consulted immediately while the case is being managed. Of notation, wounds should not be explored on the field or in the emergency department given the risk of exacerbating the wound.
Due to the advances in diagnostic imaging, management of PNI has been shifting from a "zone-based" approach, which uses anatomical site of injury to guide decisions, to a "no-zone" approach which uses a symptom-based algorithm.[25] The no-zone approach uses a hard signs and imaging arrangement to guide adjacent steps. Hard signs include airway compromise, unresponsive stupor, diminished pulses, uncontrolled bleeding, expanding hematoma, bruits/thrill, air bubbling from wound or extensive subcutaneous air, stridor/hoarseness, neurological deficits.[25] If whatsoever hard signs are present, immediate surgical exploration and repair is pursued alongside airway and bleeding control. If at that place are no difficult signs, the person receives a multi-detector CT angiography for better diagnosis. A directed angiography or endoscopy may exist warranted in a high-gamble trajectory for the gunshot. A positive finding on CT leads to operative exploration. If negative, the person may exist observed with local wound care.[25]
Chest [edit]
Of import anatomy in the breast includes the chest wall, ribs, spine, spinal string, intercostal neurovascular bundles, lungs, bronchi, middle, aorta, major vessels, esophagus, thoracic duct, and diaphragm. Gunshots to the chest can thus cause severe haemorrhage (hemothorax), respiratory compromise (pneumothorax, hemothorax, pulmonary contusion, tracheobronchial injury), cardiac injury (pericardial tamponade), esophageal injury, and nervous system injury.[26]
Initial workup as outlined in the Workup section is especially of import with gunshot wounds to the chest considering of the high risk for straight injury to the lungs, middle, and major vessels. Important notes for the initial workup specific for chest injuries are equally follows. In people with pericardial tamponade or tension pneumothorax, the breast should be evacuated or decompressed if possible prior to attempting tracheal intubation because the positive pressure ventilation can cause hypotention or cardiovascular plummet.[27] Those with signs of a tension pneumothorax (asymmetric animate, unstable blood flow, respiratory distress) should immediately receive a chest tube (> French 36) or needle decompression if chest tube placement is delayed.[27] FAST exam should include extended views into the chest to evaluate for hemopericardium, pneumothorax, hemothorax, and peritoneal fluid.[27]
Those with cardiac tamponade, uncontrolled haemorrhage, or a persistent air leak from a chest tube all crave surgery.[28] Cardiac tamponade can be identified on FAST test. Blood loss warranting surgery is 1–i.5 L of firsthand chest tube drainage or ongoing bleeding of 200-300 mL/hr.[28] [29] Persistent air leak is suggestive of tracheobronchial injury which volition not heal without surgical intervention.[28] Depending on the severity of the person's condition and if cardiac abort is recent or imminent, the person may crave surgical intervention in the emergency department, otherwise known every bit an emergency department thoracotomy (EDT).[30]
However, not all gunshot to the chest require surgery. Asymptomatic people with a normal breast X-ray tin can be observed with a repeat exam and imaging after 6 hours to ensure no delayed development of pneumothorax or hemothorax.[27] If a person but has a pneumothorax or hemothorax, a chest tube is ordinarily sufficient for management unless there is large volume bleeding or persistent air leak as noted above.[27] Boosted imaging after initial breast X-ray and ultrasound tin can be useful in guiding next steps for stable people. Common imaging modalities include chest CT, formal echocardiography, angiography, esophagoscopy, esophagography, and bronchoscopy depending on the signs and symptoms.[31]
Abdomen [edit]

Important beefcake in the belly includes the tum, small-scale bowel, colon, liver, spleen, pancreas, kidneys, spine, diaphragm, descending aorta, and other abdominal vessels and nerves. Gunshots to the abdomen tin can thus cause severe bleeding, release of bowel contents, peritonitis, organ rupture, respiratory compromise, and neurological deficits.
The most important initial evaluation of a gunshot wound to the belly is whether there is uncontrolled bleeding, inflammation of the peritoneum, or spillage of bowel contents. If any of these are present, the person should exist transferred immediately to the operating room for laparotomy.[32] If it is difficult to evaluate for those indications because the person is unresponsive or incomprehensible, it is up to the surgeon'due south discretion whether to pursue laparotomy, exploratory laparoscopy, or alternative investigative tools.
Although all people with intestinal gunshot wounds were taken to the operating room in the past, practice has shifted in recent years with the advances in imaging to non-operative approaches in more stable people.[33] If the person's vital signs are stable without indication for firsthand surgery, imaging is done to determine the extent of injury.[33] Ultrasound (FAST) and assist identify intra-intestinal haemorrhage and X-rays can help determine bullet trajectory and fragmentation.[33] Yet, the best and preferred manner of imaging is high-resolution multi-detector CT (MDCT) with IV, oral, and sometimes rectal contrast.[33] Severity of injury found on imaging volition determine whether the surgeon takes an operative or close observational approach.
Diagnostic peritoneal lavage (DPL) has become largely obsolete with the advances in MDCT, with use limited to centers without access to CT to guide requirement for urgent transfer for operation.[33]
Extremities [edit]

Acute penetrating trauma from a shut-range shotgun blast injury to knee. Birdshot pellets are visible in the wound, within the shattered patella. The pulverization wad from the shotgun vanquish has been extracted from the wound, and is visible at the upper correct of the image.
The iv master components of extremities are bones, vessels, nerves, and soft tissues. Gunshot wounds can thus cause severe bleeding, fractures, nerve deficits, and soft tissue impairment. The Mangled Extremity Severity Score (MESS) is used to classify the severity of injury and evaluates for severity of skeletal and/or soft tissue injury, limb ischemia, shock, and age.[34] Depending on the extent of injury, direction tin range from superficial wound care to limb amputation.
Vital sign stability and vascular assessment are the well-nigh important determinants of management in extremity injuries. As with other traumatic cases, those with uncontrolled bleeding require firsthand surgical intervention.[22] If surgical intervention is not readily available and straight pressure is insufficient to control bleeding, tourniquets or direct clamping of visible vessels may be used temporarily to slow agile haemorrhage.[35] People with difficult signs of vascular injury also require firsthand surgical intervention. Hard signs include active bleeding, expanding or pulsatile hematoma, bruit/thrill, absent-minded distal pulses and signs of extremity ischemia.[36]
For stable people without hard signs of vascular injury, an injured extremity alphabetize (IEI) should be calculated by comparing the blood pressure level in the injured limb compared to an uninjured limb in order to further evaluate for potential vascular injury.[37] If the IEI or clinical signs are suggestive of vascular injury, the person may undergo surgery or receive further imaging including CT angiography or conventional arteriography.
In improver to vascular management, people must be evaluated for os, soft tissue, and nerve injury. Plain films can be used for fractures alongside CTs for soft tissue assessment. Fractures must be debrided and stabilized, fretfulness repaired when possible, and soft tissue debrided and covered.[38] This process can ofttimes require multiple procedures over time depending on the severity of injury.
Epidemiology [edit]
In 2015, nearly a million gunshot wounds occurred from interpersonal violence.[10] Firearms, globally in 2016, resulted in 251,000 deaths upwardly from 209,000 in 1990.[5] Of these deaths 161,000 (64%) were the result of assault, 67,500 (27%) were the result of suicide, and 23,000 were accidents.[5] Firearm related deaths are almost common in males betwixt the ages of twenty to 24 years.[5]
The countries with the greatest number of deaths from firearms are Brazil, United States, Mexico, Colombia, Venezuela, Guatemala and S Africa which make up just over half the total.[5] In the United States in 2015 about half of the 44,000 people who died by suicide did so with a gun.[39]
As of 2016, the countries with the highest rates of gun violence per capita were Republic of el salvador, Venezuela, and Guatemala with xl.3, 34.8, and 26.8 violent gun deaths per 100,000 people respectively.[40] The countries with the lowest rates of were Singapore, Japan, and South Korea with 0.03, 0.04, and 0.05 fierce gun deaths per 100,000 people respectively.[forty]
Canada [edit]
In 2016, near 893 people died due to gunshot wounds in Canada (two.1 per 100,000).[5] Well-nigh eighty% were suicides, 12% were assaults, and four% percent were an blow.[41]
Usa [edit]
In 2017, there were 39,773 deaths in the The states as a result gunshot wounds.[15] Of these 60% were suicides, 37% were homicides, i.4% were by police enforcement, i.two% were accidents, and 0.nine% were from an unknown cause.[xv] This is upwardly from 37,200 deaths in 2016 due to a gunshot wound (10.6 per 100,000).[5] With respect to those that pertain to interpersonal violence, it had the 31st highest charge per unit in the world with three.85 deaths per 100,000 people in 2016.[40] The majority of all homicides and suicides are firearm-related, and the bulk of firearm-related deaths are the outcome of murder and suicide.[42] When sorted by Gdp, withal, the United States has a much higher vehement gun death rate compared to other developed countries, with over 10 times the number of firearms assail deaths than the next 4 highest Gdp countries combined.[43] Gunshot violence is the third most costly cause of injury and the 4th almost expensive form of hospitalization in the United States.[44]
History [edit]
Until the 1880s, the standard practice for treating a gunshot wound called for physicians to insert their unsterilized fingers into the wound to probe and locate the path of the bullet.[45] Standard surgical theory such equally opening abdominal cavities to repair gunshot wounds,[46] germ theory, and Joseph Lister's technique for antiseptic surgery using diluted carbolic acid, had non even so been accepted as standard practice. For example, sixteen doctors attended to President James A. Garfield after he was shot in 1881, and most probed the wound with their fingers or dirty instruments.[47] Historians concur that massive infection was a significant factor in Garfield's death.[45] [48]
At near the same fourth dimension, in Tombstone, Arizona Territory, on 13 July 1881, George E. Goodfellow performed the first laparotomy to treat an intestinal gunshot wound.[49] : M-9 Goodfellow pioneered the use of sterile techniques in treating gunshot wounds,[50] washing the person'south wound and his easily with lye soap or whisky, and his patient, dissimilar the President, recovered.[51] He became America's leading say-so on gunshot wounds[52] and is credited every bit the United states' starting time civilian trauma surgeon.[53]
Mid-nineteenth-century handguns such equally the Filly revolvers used during the American Civil War had muzzle velocities of simply 230–260 g/southward and their pulverization and brawl predecessors had velocities of 167 m/s or less. Unlike today's high-velocity bullets, nineteenth-century balls produced almost little or no cavitation and, being slower moving, they were liable to social club in unusual locations at odds with their trajectory.[54]
Wilhelm Röntgen'south discovery of 10-rays in 1895 led to the use of radiographs to locate bullets in wounded soldiers.[55]
Survival rates for gunshot wounds improved among United states military personnel during the Korean and Vietnam Wars, due in role to helicopter evacuation, along with improvements in resuscitation and battlefield medicine.[55] [56] Similar improvements were seen in Us trauma practices during the Iraq War.[57] Some war machine trauma care practices are disseminated by citizen soldiers who return to civilian practice.[55] [58] [59] 1 such practice is to transfer major trauma cases to an operating theater equally soon as possible, to end internal haemorrhage. Within the United states, the survival rate for gunshot wounds has increased, leading to apparent declines in the gun death rate in states that have stable rates of gunshot hospitalizations.[threescore] [61] [62] [63]
Research [edit]
Enquiry into gunshot wounds in the USA is hampered past lack of funding. Federal-funded research into firearm injury, epidemiology, violence, and prevention is minimal.
See as well [edit]
- Stab wound, an equivalent penetrating injury caused by a bladed weapon or any other precipitous objects.
- Blast injury, an injury that may present similar dangers to a gunshot wound.
References [edit]
- ^ a b c "Gun Shot Wounds - Trauma - Orthobullets". world wide web.orthobullets.com . Retrieved thirteen July 2019.
- ^ a b c d "Gunshot wounds - aftercare: MedlinePlus Medical Encyclopedia". medlineplus.gov . Retrieved 13 July 2019.
- ^ Stein, JS; Strauss, E (January 1995). "Gunshot wounds to the upper extremity. Evaluation and management of vascular injuries". The Orthopedic Clinics of North America. 26 (ane): 29–35. doi:10.1016/S0030-5898(20)31965-9. PMID 7838501.
- ^ Nair, R.; Abdool-Carrim, A. T.; Robbs, J. 5. (2000). "Gunshot injuries of the popliteal artery - Nair - 2000 - BJS - Wiley Online Library". The British Periodical of Surgery. 87 (v): 602–seven. doi:x.1046/j.1365-2168.2000.01397.x. PMID 10792317. S2CID 8418598.
- ^ a b c d e f k h i j yard 50 m Global Burden of Disease 2016 Injury, Collaborators.; Naghavi, M; Marczak, LB (28 August 2018). "Global Mortality From Firearms, 1990-2016". JAMA. 320 (viii): 792–814. doi:10.1001/jama.2018.10060. PMC6143020. PMID 30167700.
- ^ a b Branas, CC; Han, Southward; Wiebe, DJ (2016). "Booze Use and Firearm Violence". Epidemiologic Reviews. 38 (1): 32–45. doi:10.1093/epirev/mxv010. PMC4762248. PMID 26811427.
- ^ a b Lee, LK; Fleegler, EW; Farrell, C; Avakame, Due east; Srinivasan, S; Hemenway, D; Monuteaux, MC (ane January 2017). "Firearm Laws and Firearm Homicides: A Systematic Review". JAMA Internal Medicine. 177 (1): 106–119. doi:10.1001/jamainternmed.2016.7051. PMID 27842178. S2CID 205119294.
- ^ a b Santaella-Tenorio, J; Cerdá, G; Villaveces, A; Galea, S (2016). "What Do Nosotros Know Well-nigh the Association Betwixt Firearm Legislation and Firearm-Related Injuries?". Epidemiologic Reviews. 38 (1): 140–57. doi:10.1093/epirev/mxv012. PMC6283012. PMID 26905895.
- ^ a b c Breeze, John; Penn-Barwell, Jowan G.; Keene, Damian; O'Reilly, David; Jeyanathan, Jeyasankar; Mahoney, Peter F. (2017). Ballistic Trauma: A Applied Guide (four ed.). Springer. p. 75. ISBN9783319613642.
- ^ a b c GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic assay for the Global Burden of Affliction Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(sixteen)31678-6. PMC5055577. PMID 27733282.
- ^ "Gunshot wound definition and pregnant | Collins English Dictionary". www.collinsdictionary.com . Retrieved 13 July 2019.
- ^ a b "Gunshot Injuries; Gunshot wounds (GSW) information". patient.info . Retrieved 13 July 2019.
- ^ Aaron, DL; Fadale, PD; Harrington, CJ; Born, CT (May 2011). "Posttraumatic stress disorders in civilian orthopaedics". The Journal of the American Academy of Orthopaedic Surgeons. xix (five): 245–50. doi:10.5435/00124635-201105000-00001. PMID 21536623. S2CID 29498901.
- ^ Cukier, West; Eagen, SA (Feb 2018). "Gun violence". Current Opinion in Psychology. xix: 109–112. doi:10.1016/j.copsyc.2017.04.008. PMID 29279206.
- ^ a b c d e f McLean, Robert M.; Harris, Patrice; Cullen, John; Maier, Ronald V.; Yasuda, Kyle E.; Schwartz, Bruce J.; Benjamin, Georges C. (7 August 2019). "Firearm-Related Injury and Death in the Us: A Call to Action From the Nation's Leading Physician and Public Wellness Professional Organizations". Register of Internal Medicine. 171 (eight): 573–577. doi:10.7326/M19-2441. PMID 31390463.
- ^ Rhee, PM; Moore, EE; Joseph, B; Tang, A; Pandit, V; Vercruysse, M (June 2016). "Gunshot wounds: A review of ballistics, bullets, weapons, and myths". The Journal of Trauma and Astute Care Surgery. 80 (vi): 853–67. doi:10.1097/TA.0000000000001037. PMID 26982703.
- ^ Lamb, C. M.; Garner, J. P. (Apr 2014). "Selective non-operative direction of noncombatant gunshot wounds to the belly: a systematic review of the show". Injury. 45 (four): 659–666. doi:ten.1016/j.injury.2013.07.008. ISSN 1879-0267. PMID 23895795.
- ^ a b c d Maiden, Nicholas (September 2009). "Ballistics reviews: mechanisms of bullet wound trauma". Forensic Science, Medicine, and Pathology. 5 (3): 204–209. doi:10.1007/s12024-009-9096-6. PMID 19644779. S2CID 34589917.
...the temporary cavity is the most important cistron in wound ballistics of loftier velocity burglarize bullets...the importance of the temporary cavity is recognized by all other contemporary researchers...The temporary crenel also has little or no wounding potential with handgun bullets because the corporeality of kinetic free energy deposited in the tissue is insufficient to cause remote injuries. The size of the temporary cavity is approximately proportional to the kinetic energy of the striking bullet and also the amount of resistance the tissue has to stress.
- ^ a b c d eastward Rhee, Peter 1000.; Moore, Ernest E.; Joseph, Bellal; Tang, Andrew; Pandit, Viraj; Vercruysse, Gary (one June 2016). "Gunshot wounds: A review of ballistics, bullets, weapons, and myths". The Journal of Trauma and Acute Intendance Surgery. eighty (6): 853–867. doi:10.1097/TA.0000000000001037. ISSN 2163-0755. PMID 26982703.
- ^ Hanna, Tarek N.; Shuaib, Waqas; Han, Tatiana; Mehta, Ajeet; Khosa, Faisal (i July 2015). "Firearms, bullets, and wound ballistics: An imaging primer". Injury. 46 (vii): 1186–1196. doi:10.1016/j.injury.2015.01.034. PMID 25724396.
Each bullet has its intrinsic mass, just the initial velocity is largely a function of the firearm. Due to short barrel length, handguns produce a low-velocity projectile that normally deposits all of its kinetic energy within the target, thus creating an entry but no exit wound. Rifles take longer barrel lengths that produce a high velocity, high-energy projectile.
- ^ "Gun Shot Wounds - Trauma - Orthobullets". world wide web.orthobullets.com . Retrieved 28 March 2020.
- ^ a b c Advanced Trauma Life Support (ATLS) Student Course Manual (9th ed.). American College of Surgeons. 2012. ISBN978-1880696026.
- ^ Shiroff, AM; Gale, SC; Martin, ND; Marchalik, D; Petrov, D; Ahmed, HM; Rotondo, MF; Gracias, VH (January 2013). "Penetrating neck trauma: a review of management strategies and discussion of the 'No Zone' approach". The American Surgeon. 79 (1): 23–nine. doi:10.1177/000313481307900113. PMID 23317595. S2CID 23436327.
- ^ a b Tisherman, Samuel A.; Bokhari, Faran; Collier, Bryan; Cumming, John; Ebert, James; Holevar, Michele; Kurek, Stanley; Leon, Stuart; Rhee, Peter (1 May 2008). "Clinical Practise Guideline: Penetrating Zone Two Neck Trauma". The Periodical of Trauma: Injury, Infection, and Disquisitional Intendance. 64 (5): 1392–1405. doi:ten.1097/ta.0b013e3181692116. ISSN 0022-5282. PMID 18469667.
- ^ a b c Shiroff, Adam M.; Gale, Stephen C.; Martin, Niels D.; Marchalik, Daniel; Petrov, Dmitriy; Ahmed, Hesham G.; Rotondo, Michael F.; Gracias, Vicente H. (January 2013). "Penetrating neck trauma: a review of management strategies and give-and-take of the 'No Zone' arroyo". The American Surgeon. 79 (one): 23–29. doi:10.1177/000313481307900113. ISSN 1555-9823. PMID 23317595. S2CID 23436327.
- ^ Marx, John; Walls, Ron; Hockberger, Robert (1 August 2013). Rosen's emergency medicine : concepts and clinical do. Marx, John A.,, Hockberger, Robert Due south.,, Walls, Ron M.,, Biros, Michelle H.,, Danzl, Daniel F.,, Gausche-Colina, Marianne (Eighth ed.). Philadelphia, PA. ISBN9781455749874. OCLC 853286850.
- ^ a b c d eastward Karmy-Jones, Riyad; Namias, Nicholas; Coimbra, Raul; Moore, Ernest E.; Schreiber, Martin; McIntyre, Robert; Croce, Martin; Livingston, David H.; Sperry, Jason 50. (Dec 2014). "Western Trauma Clan critical decisions in trauma: penetrating chest trauma". The Journal of Trauma and Astute Care Surgery. 77 (6): 994–1002. doi:x.1097/TA.0000000000000426. ISSN 2163-0763. PMID 25423543.
- ^ a b c Meredith, J. Wayne; Hoth, J. Jason (February 2007). "Thoracic trauma: when and how to intervene". The Surgical Clinics of North America. 87 (1): 95–118, vii. doi:10.1016/j.suc.2006.09.014. ISSN 0039-6109. PMID 17127125.
- ^ Karmy-Jones, Riyad; Jurkovich, Gregory J. (March 2004). "Blunt chest trauma". Current Issues in Surgery. 41 (3): 211–380. doi:10.1016/j.cpsurg.2003.12.004. PMID 15097979.
- ^ Burlew, Clay Cothren; Moore, Ernest East.; Moore, Frederick A.; Coimbra, Raul; McIntyre, Robert C.; Davis, James W.; Sperry, Jason; Biffl, Walter 50. (December 2012). "Western Trauma Association critical decisions in trauma: resuscitative thoracotomy". The Journal of Trauma and Acute Care Surgery. 73 (vi): 1359–1363. doi:x.1097/TA.0b013e318270d2df. ISSN 2163-0763. PMID 23188227.
- ^ Mirvis, Stuart East. (April 2004). "Diagnostic imaging of acute thoracic injury". Seminars in Ultrasound, CT and MRI. 25 (2): 156–179. doi:10.1016/j.sult.2004.02.001. PMID 15160796.
- ^ Jansen, Jan O.; Inaba, Kenji; Resnick, Shelby; Fraga, Gustavo P.; Starling, Sizenando V.; Rizoli, Sandro B.; Boffard, Kenneth D.; Demetriades, Demetrios (May 2013). "Selective not-operative direction of abdominal gunshot wounds: survey of practice". Injury. 44 (5): 639–644. doi:10.1016/j.injury.2012.01.023. PMID 22341771.
- ^ a b c d e Pryor, John P.; Reilly, Patrick M.; Dabrowski, Thou. Paul; Grossman, Michael D.; Schwab, C. William (March 2004). "Nonoperative management of intestinal gunshot wounds". Annals of Emergency Medicine. 43 (three): 344–353. doi:10.1016/s0196-0644(03)00815-one. PMID 14985662.
- ^ Johansen, K.; Daines, M.; Howey, T.; Helfet, D.; Hansen, S. T. (May 1990). "Objective criteria accurately predict amputation post-obit lower extremity trauma". The Journal of Trauma. 30 (five): 568–572, discussion 572–573. doi:10.1097/00005373-199005000-00007. PMID 2342140.
- ^ Play a trick on, Nicole; Rajani, Ravi R.; Bokhari, Faran; Chiu, William C.; Kerwin, Andrew; Seamon, Mark J.; Skarupa, David; Frykberg, Eric; Eastern Association for the Surgery of Trauma (Nov 2012). "Evaluation and management of penetrating lower extremity arterial trauma: an Eastern Association for the Surgery of Trauma do management guideline". The Periodical of Trauma and Acute Care Surgery. 73 (v Suppl iv): S315–320. doi:ten.1097/TA.0b013e31827018e4. PMID 23114487.
- ^ "National Trauma Data Bank 2012 Annual Report". American Higher of Surgeons 8.
- ^ "WESTERN TRAUMA ASSOCIATION". westerntrauma.org. Archived from the original on 22 September 2018. Retrieved 21 March 2018.
- ^ "Management of Complex Extremity Trauma". American College of Surgeons Committee on Trauma. Archived from the original on 29 August 2017. Retrieved 21 March 2018.
- ^ Houtsma, C; Butterworth, SE; Anestis, Dr. (August 2018). "Firearm suicide: pathways to hazard and methods of prevention". Current Stance in Psychology. 22: seven–xi. doi:10.1016/j.copsyc.2017.07.002. PMID 30122279. S2CID 52040180.
- ^ a b c "GBD Compare | IHME Viz Hub". vizhub.healthdata.org . Retrieved 14 March 2018.
- ^ Government of Canada, Section of Justice (ten March 1999). "Firearms, Accidental Deaths, Suicides and Violent Crime: An Updated Review of the Literature with Special Reference to the Canadian Situation". world wide web.justice.gc.ca . Retrieved 13 July 2019.
- ^ Wellford, Charles F.; Pepper, John V.; Petrie, Carol V. (2005). Firearms and violence: A disquisitional review (Written report). National Research Council. Commission to Improve Research Information and Data on Firearms.
- ^ Marczak, Laurie; O'Rourke, Kevin; Shepard, Dawn; Leach-Kemon, Katherine; Evaluation, for the Institute for Health Metrics and (13 December 2016). "Firearm Deaths in the United States and Globally, 1990-2015". JAMA. 316 (22): 2347. doi:10.1001/jama.2016.16676. ISSN 0098-7484. PMID 27959984.
- ^ Lichte, Philipp; Oberbeck, Reiner; Binnebösel, Marcel; Wildenauer, Rene; Pape, Hans-Christoph; Kobbe, Philipp (17 June 2010). "A noncombatant perspective on ballistic trauma and gunshot injuries". Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. xviii (35): 35. doi:10.1186/1757-7241-eighteen-35. PMC2898680. PMID 20565804.
- ^ a b Schaffer, Amanda (25 July 2006). "A president felled past an assassin and 1880s medical care". The New York Times. New York, New York. Retrieved 29 April 2016.
- ^ Crane, Michael A. (2003). "Dr. Goodfellow: gunfighter'south surgeon" (PDF). Archived from the original (PDF) on nineteen October 2013. Retrieved x March 2013.
- ^ "The expiry of President Garfield, 1881". Retrieved 11 March 2013.
- ^ Rutkow, Ira (2006). James A. Garfield. New York: Macmillan Publishers. ISBN978-0-8050-6950-1. OCLC 255885600.
- ^ Charles E. Sajous, ed. (1890). Almanac of the Universal Medical Sciences And Analytical Index 1888-1896. Vol. 3. Philadelphia: F.A. Davis Company.
- ^ "Come up face to face with history" (PDF). Cochise County. pp. 8–nine. Archived from the original (PDF) on 17 June 2013.
- ^ Edwards, Josh (2 May 1980). "George Goodfellow's medical treatment of tummy wounds became legendary". The Prescott Courier. pp. 3–5.
- ^ "Dr. George Goodfellow". Archived from the original on 20 December 2014. Retrieved 8 March 2013.
- ^ "Tombstone's doctor famous every bit surgeon". The Prescott Courier. 12 September 1975. Retrieved 11 March 2013.
- ^ Kennerk, Barry (Dec 2011). "In Danger and Distress - Presentation of Gunshot Cases to Dublin Hospitals during the Meridian of Fenianism, 1866-187". Social History of Medicine. Oxford University Press. 24 (three): 588–607. doi:10.1093/shm/hkq094. ISSN 0951-631X.
- ^ a b c Manring MM, Militarist A, Calhoun JH, Andersen RC (2009). "Treatment of state of war wounds: a historical review". Clin Orthop Relat Res. 467 (8): 2168–91. doi:ten.1007/s11999-009-0738-5. PMC2706344. PMID 19219516.
- ^ "Chapter 3 - Medical Back up 1965-1970". Archived from the original on 6 June 2016. Retrieved 13 June 2016.
- ^ Service, Lee Bowman, Scripps Howard News (16 March 2013). "Iraq War 10-year anniversary: Survival charge per unit of wounded soldiers meliorate than previous wars". Archived from the original on iv September 2018. Retrieved 13 June 2016.
- ^ "Military medical techniques saving lives at domicile". GOV.UK.
- ^ "The part of the gun in the advocacy of medicine". 8 January 2015. Archived from the original on vi January 2018. Retrieved 13 June 2016.
- ^ Jena, Anupam B.; Sun, Eric C.; Prasad, Vinay (2014). "Does the Failing Lethality of Gunshot Injuries Mask a Rising Epidemic of Gun Violence in the United States?". Journal of General Internal Medicine. 29 (7): 1065–1069. doi:ten.1007/s11606-014-2779-z. ISSN 0884-8734. PMC4061370. PMID 24452421.
- ^ "Lower murder rate linked to medical advance, not less violence".
- ^ Fields, Gary; McWhirter, Cameron (8 December 2012). "In Medical Triumph, Homicides Autumn Despite Soaring Gun Violence". Wall Street Journal.
- ^ "Murder and Medicine - The Lethality of Criminal Attack 1960-1999" (PDF). www.universitychurchchicago.org.
External links [edit]
- Virtual Autopsy – CT scans of fatal gunshot wounds
- Patient.info
Source: https://en.wikipedia.org/wiki/Gunshot_wound
0 Response to "what to do if you get shot by a gun"
Post a Comment